Therapeutic Hypothermia 101: Cooling Patients, Breaking Barriers, And The Legendary Code Brown
Here I reminisce about my evolution in cooling comatose patients, making groundbreaking protocols, and the unforgettable day a “code brown” changed everything in the ICU.
Folks, I’m deep in the trenches working on a series of posts that might be my most important yet. I genuinely believe I’ve uncovered a game-changing therapy for a wide range of chronic diseases (and no, I haven’t been drinking!). This upcoming series will raise awareness about a treatment with a huge potential to protect health and tackle illness—a breakthrough that’s still flying under the radar and sorely overlooked in research circles (as well as among the MAHA crowd and the wider “alternative” health provider community).
So, hang in and hold on, I would strongly suggest you subscribe now not to miss it, but while I am on this writing “sabbatical,” I thought I would entertain you with some fun and/or interesting excerpts from previous posts that I re-wrote. Enjoy.
In a post I wrote long ago, I recounted my somewhat prolonged and arduous path into medical school, followed by residency and fellowship training. I followed that post with a review of the therapies I did “deep dives” of research into during my academic career.
Today, I thought I would highlight the first “rabbit hole” I ever went down in my academic career, searching for innovative approaches to healing the human body in illness. That first foray was my research into something called therapeutic hypothermia, a highlight of which was a “Code Brown” incident that all involved will never forget (for those in health care, you know what a Code Brown is).
After I completed my training, I took a position as a clinician-educator at the teaching hospital where I had done my subspecialty fellowship training (Beth Israel Medical Center in lower Manhattan). It is always an honor when those who trained you.. end up hiring you as a partner. Picture of me when I joined the Pulmonary and Critical Care Division in 2008 :). A little slimmer apparently, yeesh.
Anyway, one of the proudest achievements in my career as a “clinician-educator” was becoming one of the youngest Program Directors (PDs) of a Pulmonary and Critical Care Fellowship Training Program in the country (which is relevant to this account).
However, what I am most proud of from that time was helping pioneer two different, then novel fields of my specialty - the first was on the study and application of therapeutic hypothermia in post-cardiac arrest patients, and the other was in creating and teaching a novel diagnostic approach to critical illness using “point-of-care ultrasonography.” Today, I will share with you my introduction to and experiences with the therapy that was then called “Mild Therapeutic Hypothermia” (now it is called “Targeted Temperature Management”).
Therapeutic Hypothermia
My interest in therapeutic hypothermia developed in 2005 when I was still a fellow in training. It stemmed from a case of a patient who had suffered cardiac arrest on one of the hospital wards. We successfully resuscitated and brought him back to the ICU, but, as is typical, he remained in a dense coma with little detectable brain function. The downtime of the arrest was almost 30 minutes, his initial rhythm was PEA, both of which are really, really not good prognostically for achieving neurologically intact survival.
I was by the nurses station when suddenly, my first mentor Dr. Paul Mayo, told me that we should “cool him.”
I asked why, and he replied that he had seen some papers on it and that the Europeans were starting to do this to comatose post-arrest patients. I learned later that they did this to cool their brain cells, the intent being to lower metabolic activity, preserve cellular function, and inhibit an inflammatory attack from elsewhere (today, I would just bathe his head in DMSO while running an IV drip… obviously).
Anyway, we cooled him, and three days later… he regained full consciousness. We actually got him quite cold, purposefully overshooting the non-consensus, but often used 33 °C (91.4°F). I think we went for 28 °C (82.4°F), but don’t quote me on that. Although I will skip a summary of my many early lectures on this topic, I will pull a few cool, historical “fun-facts:”
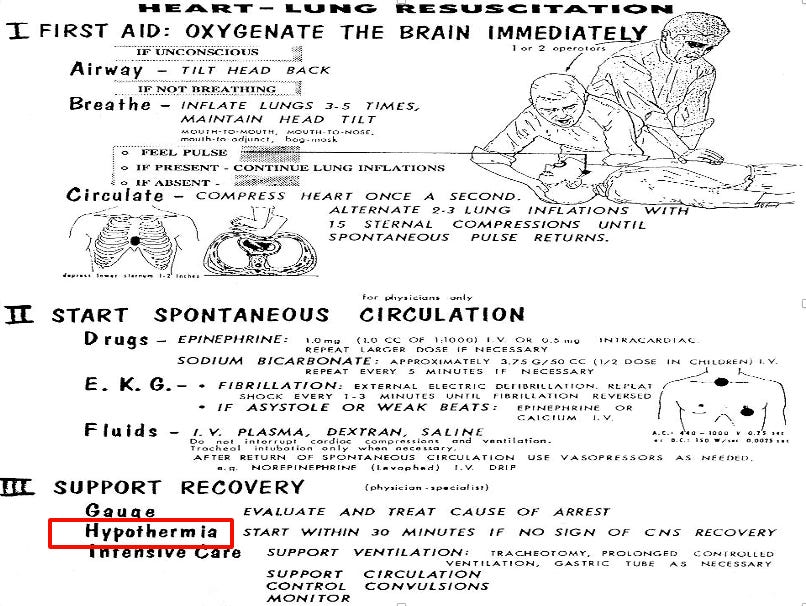
Peter Safar: Did you know that in one of the earliest monographs on how to do CPR (1961), from literally the founder of both CPR and ICU, a guy named Safar in Pittsburgh, had put post-arrest hypothermia as part of the protocol?
It quickly disappeared, though, due to concerns over side effects and the technological challenges of delivering the therapy, and thus became “A Forgotten Side Of Medicine” (as you will learn, I was one of, if not the, guy who resurrected it in NYC). AMD would be proud :).
I gotta say that I must take a moment to say a few words about Dr. Peter Safar who was an absolute LEGEND (to me anyway)
Dr. Peter Safar (1924–2003), was an Austrian-American anesthesiologist. He is widely recognized as the "Father of CPR" for developing the modern approach to cardiopulmonary resuscitation. Dr. Safar also established the first intensive care unit (ICU) in the United States and played a critical role in creating and standardizing the modern ambulance and emergency medical services system.
Basically, Safar invented CPR, ICU’s, and the ambulance system. I cannot imagine how many millions of people around the world are now alive as a result of his innovations.
Baron Dominique-Jean Larrey - Napoleon’s chief army surgeon and a legendary innovator in battlefield medicine.
Larrey noticed that soldiers who had suffered cold injuries (like frostbite) and were brought close to the campfires often developed gangrene and died, while those who were left farther from the fire and allowed to warm up very slowly were more likely to survive (note that officers typically were allowed places closer to the fire while infantrymen were farther away).
Although his observations did not directly relate to the mechanisms of benefit of MTH on the brain (it was more on how to treat hypothermia by gradual re-warming), his insights were ahead of his time and laid the groundwork for what we now recognize as modern hypothermia care.
Anyway, it was after this clinical experience that I delved into researching everything known about the therapy. Wait, another fun fact about my first case that I just remembered. The patient had COPD and a close colleague was his pulmonologist, who later told me that the guy was one of the crabbiest, rudest, most unpleasant patients he had ever taken care of (that’s saying a lot for NYC) Before his arrest, that is. After he became much more docile and even pleasant.
Anyway, my “advocacy” for therapeutic hypothermia became first clinical initiative that I ever led. I created and instituted my hospital’s first therapeutic hypothermia protocol. As a result, I quickly became a regional and national expert in the therapy and started to get invited to give lectures everywhere (which taught me how to give lectures!).
I was one of the expert panel members who helped develop NYC’s “Project Hypothermia,” where, when we started, my hospital was the only one out of the 46 NYC area hospitals that had an active post-arrest hypothermia protocol.
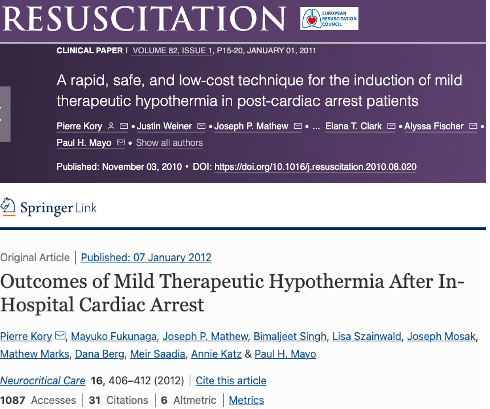
Within a few years, such protocols had been implemented at every NYC hospital, and all ambulances and paramedics were equipped and trained to start cooling post-cardiac arrest patients. I then did research studies trying to find which patients benefited most or not at all, and on whether the speed or depth of cooling mattered, etc (I was the first to do a controlled study on in-hospital cardiac arrest patients, and I also published on the rapidity of cooling using numerous techniques).
Did The Rate Of Cooling Matter?
Initially, Paul Mayo and I believed that the faster we lowered a patient's temperature, the better the outcomes would be (although we knew it was safe to do so, we later found out this was not true). But, at the time, thinking speed was critical to their survival, we adopted an aggressive, rapid-cooling protocol which we “borrowed” from the techniques used to cool Muslim pilgrims suffering heat stroke during their annual pilgrimage to Mecca.
The pilgrims are whisked into treatment units where they are disrobed, placed into hammocks, and exposed to high-speed fans while being sprayed with warm water. Why warm water? Well, if you cover them with warm water under high-speed fanning, the water evaporates faster, and this evaporative process sucks heat from the body much quicker than if you used cold water (cold water causes the surface blood vessels to constrict, thus paradoxically trapping heat).
Paul had used the same technique to cool a Polish construction worker who had suffered severe heat stroke the summer before (109F on arrival), so we employed the same method to cool our cardiac arrest patients.
Anytime we admitted a post-cardiac arrest patient, my entire ICU team would wheel in this huge industrial fan which we placed at the foot of the bed. We would strip the patient naked, and my residents would dip towels in lukewarm water and “paint” the patient with the wet towels under a super loud fan, which emitted a terrific racket.
At the same time, other residents (or students) would cool bags of saline fluids and infuse them through large IV catheters in the neck or groin, sometimes getting 2 liters of iced saline into them in ten minutes using pressure bags. Lastly, we would have two doctors do iced gastric lavages by placing a nasogastric tube in the stomach, and using a comically large syringe, they would push iced water down the tube into the stomach.
They would instill 500ml and then suck it out, then refill with iced saline, repeat. Using this “combination therapy” protocol, we achieved some of the fastest decreases in body temperature of any method known. Below is my paper shouting to the ICU world about how the fastest (and dumbest) way to cool a patient was:
As you can see below, ours wasn’t the fastest method, but it was the cheapest and fastest (and again, dumbest) method in medical history :)
Cooling patients like that was wild. One problem though, was that it created a colossal mess with puddles of water all around the bed and folks slipping, etc.
The sloppiness of the method was becoming an issue, plus it was massively labor-intensive while trying to care for 16-20 critically ill patients a day. As the leader of the hypothermia program, my hospital asked me to choose a cooling device to purchase for use in patients that was a little less chaotic, labor-intensive, and messy. There were a number of cooling devices on the market.. and I chose the one that was fastest. A device called the “Thermosuit,” which was literally an inflatable bathtub:
Basically, you unroll this sheet of plastic on the bed, place the patient in the middle, and then you inflate it. Once the bathtub was fully inflated, you put a plastic cover over it, attached the tub via hoses to a large reservoir of iced water, and a pump would propel the ice water into the bathtub via tiny holes in the top sheet, which sprayed the entire body almost like a fine sprinkler.
Problem: It was glitchy. We would have different “failures” in the process every few times we used it. My fellows began to complain when they had to cool a patient, as it was rarely a “turn-key” process.
The Code Brown Incident
I came to work one Saturday and the fellow who had been on call overnight barged into my office, telling me she was never ever going to use that stupid Thermosuit again. Basically, she had to attend to a “Code Brown” the night before. And not just any Code Brown,but a massive one (note that ICU fellows are not typically called for Code Browns (right nurses?), mostly Code Blues (arrests), Reds (massive bleeds), and RRT’s (Rapid Response emergency team calls).
Anyway, she told me that while she was trying to cool a post-arrest comatose patient at like 3 in the morning, their physiologic response was to have a massive, very watery bowel movement. While in the tub. Not good.
Then, while trying to transfer the patient out of the tub, the tub apparently deflated partly, and a river of brown spilled over the sides of the bed and all over the floor (and some of the staff). I was not there at the time.. but the fellow and nurses that were on that night never let me forget about it.
Fun Fact: Joe Varon, one of the other founders of the FLCCC, was an even earlier “hypothermiac” in our specialty. I didn’t know him then, but I had come across this picture of him early in my career, and I used to display it in my lectures (this was before I later would meet him and partner with him in forming the FLCCC). Check out his method of cooling. No wonder we would later become FLCCC brothers.
After the infamous “code brown” incident, I very quickly petitioned for the purchase of a more practical, easy-to-use device (plus by this time, I had learned that speed of cooling was less important than duration). We quickly purchased cooling pads like the ones below and never used the Thermosuit again. See? We evolve with data and clinical experience, setting new “standards of care” along the way :).
Ultimately, as more and more studies were done, my interests and expertise in therapeutic hypothermia waned as I discovered that it was largely beneficial mostly in witnessed out-of-hospital cardiac arrest patients of primary cardiac causes and not in my general ICU patients. Subsequent studies have shown that cooling such patients is less important than simply preventing temperature rises; therefore, cooling approaches are now more reactive than proactive and essentially target normothermia. However, it was a great early experience in my career (except for the code brown part :).
If you can afford to, and appreciate the time, research, and care I invest in crafting these posts (and Op-Ed’s), please support my work with a paid subscription:









Code Brown: what happens in hospitals should stay in hospitals so I’m told by my family. My wife, an RN, and I used to discuss medical care at the dinner table. Never noticed the kids were not finishing their meals until a visiting cousin literally gagged and left the table. Stool transplants were just too much I guess….;-)
My father had his head beaten in during a robbery gone wrong at a store in 1963. Bits of skull on the floor. Luckily found quickly and taken to Stanford, they tried what was said to be a pioneering treatment of putting him on a bed of ice water, as his head swelled up like a pumpkin. The nurses did not think he would survive, apparently, so never fastened his restraints. One day after a couple of months in coma, he stood up and fell over. Stanford bought him front caps. His memories seemed to have been wiped except for childhood, but he retained speech. Took years to complete his final year of university. Probably years beyond that just to become mostly functional. He did live a full life, though, all things considered - and he helped a lot of people in his career.
In a freak accident last April, he slipped on outdoor stairs and flew several feet before landing on his head, on the same side, not far from the old injury. Was not found for an hour, intubated by ambulance, brain bounce caused several hemorrhages and brain stem injury, so of course the medics were not confident. This time he was treated with heavy sedatives and a ventilator. Very health for age and on no medications, he developed a respiratory infection which was not treated perhaps because the assumption was that he probably would not make it. Interestingly, once the sedatives were dialed down after a week, he began responding to commands to move feet and hands, lifting his arms to help with bathing, and opening eyes. In assessing what the prognosis might be, the interesting thing was that the previous area of injury in the brain seemed to have formed a barrier which prevented one area of hemorrhage from seeping further into the brain, almost in a protective way. I would like to say there was a chance to let him recuperate, but he was given a few days to show further signs of improvement while the sedatives were lower, and he did not adequate any tricks, so it was decided that end of life care should begin. The sedatives were turned up again in anticipation of the day the machines would be turned off which was 17 days after the fall. There was breathing without the intubation, but the lungs seemed absolutely engulfed. They slurped like a sump pump in a flooded basement during the final breaths. Oxygen saturation plummeted over 15-20 minutes. I began to think there never would have been a way to survive this; after all, the policy seems to be now that after two weeks, patient has to have a tracheostomy, and families are told with tracheostomy, they can no longer be in ICU, no longer receiving suction, so therefore may decline in an alive but not thriving state… However, I can’t help but wonder if he’d have fared better from the beginning under the care of doctors from previous eras. Sorry for the heavy story. Just reminds us that we need to keep the dialogue open so that knowledge is not lost.